SHILLONG:
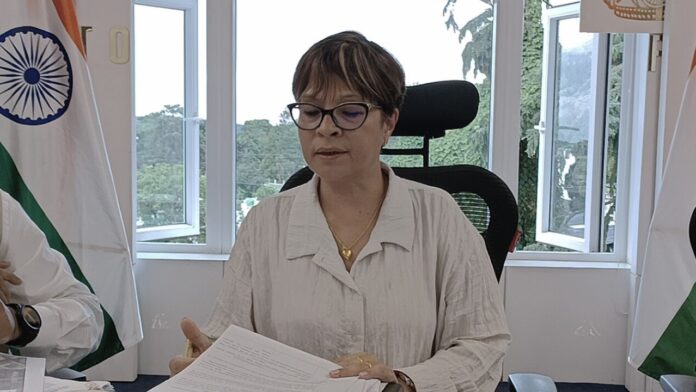
Health Minister in-charge Health & Family Welfare Ampareen Lyngdoh on Tuesday said over 1,375 cancer patients got treatment under the Megha Health Insurance Scheme (MHIS) for the period of January-August 2023.
She said 528 are females and 847 are males.
Replying to a short duration discussion in the Assembly, Lyngdoh said MHIS Phase 6 – Pradhan Mantri Jan Arogya Yojana (PMJAY) started on September 1, 2022.
Transition to the scheme’s next phase was made without any breaks and disruption, which allows beneficiaries to continue availing services under the scheme.
“Despite the change of Phase 5 to Phase 6, registered beneficiaries/households will not be required to register themselves again, therefore relieving the public from renewal of cards from one phase to the next. Such improvements in the scheme’s implementation are what contribute to the success of the scheme,” she said.
She informed that the Reliance General Insurance Company Limited is the current insurance company identified for implementing the scheme in Meghalaya for MHIS 6 which was selected through a rigorous and competitive bidding process.
Highlighting some of the key features of MHIS 6 – PMJAY, Lyngdoh said there is an increased insurance cover of Rs 5,30,000 per family per year, inclusive of Rs 30,000 OPD cover, no limits on the family size and the scheme continues to cover pre-existing diseases.
She said the number of Health Benefits Packages is 2253 packages and 2665 procedures which include OPD/Day-care, OPD diagnostics, medical treatments, surgical procedures, and highend drugs packages. Existing PMJAY-MHIS Card holders will not need to register themselves, however eligible unregistered beneficiaries can undertake the registration process at designated centres. Beneficiaries can utilise the benefits at any empanelled hospital across the country.
Stating that several improvements have been further envisioned by the government during this phase, Lyngdoh said the new financial guidelines have been introduced, to enable public hospitals to manage their insurance-generated funds more efficiently to upgrade or improve their existing services and to effectively incentivize their staff based on performance.
“With the new guidelines, public hospitals will contribute a percentage of their earnings to a State Corpus Fund, which can be utilised for treating BPL and deprived beneficiaries of the state for selected high-end tertiary care, like open heart surgeries, liver and organ transplant, and treatment for rare diseases in hospitals, either inside or outside the state of Meghalaya.”
Further, the minister informed that the State Corpus Fund is an initiative to provide additional benefits to BPL/Deprived beneficiaries, over and above the existing insurance cover.
On the medical benefits to government employees, Lyngdoh said the government has adopted Meghalaya Medical Attendance Rules (MMA) 2021 under the department of health and family welfare, providing government employees with a reimbursement-based system for availing medical treatment.
The state currently has approximately 68,280 in-service employees and approximately 24,044 pensioners and all-India service employees.
Overall, approximately 4,42,155 members are getting medical reimbursements from different departments based on MMA rules 2021.
Presently, the government employees do not have cashless coverage for their medical services, despite the state having universal health coverage for all citizens.